Archived - Chapter 1
Fighting COVID-19
1.1 COVID-19 in Canada
A second wave of the COVID-19 pandemic has gripped countries and economies around the world, including Canada. COVID-19 has emerged in all provinces and territories, with a concentration of active cases in a number of provinces. By November 24, the virus had resulted in over 342,000 diagnosed cases and, tragically, more than 11,600 deaths here in Canada.
1.1.1 Virus Resurgence in Canada
After significantly bringing down cases with spring lockdowns, Canada re-opened over the summer. The fall has brought a resurgence of the virus and community transmission in Canada. Since the end of August, the average number of daily new cases across Canada has increased tenfold from a plateau of fewer than 500 cases to over 5,000 cases as of November 24 (Chart 1.1). Recent modelling has projected that if Canadians do not reduce their contacts, Canada could face 20,000 new cases a day by late December.
New Cases and Deaths of COVID-19 (7-day moving average)
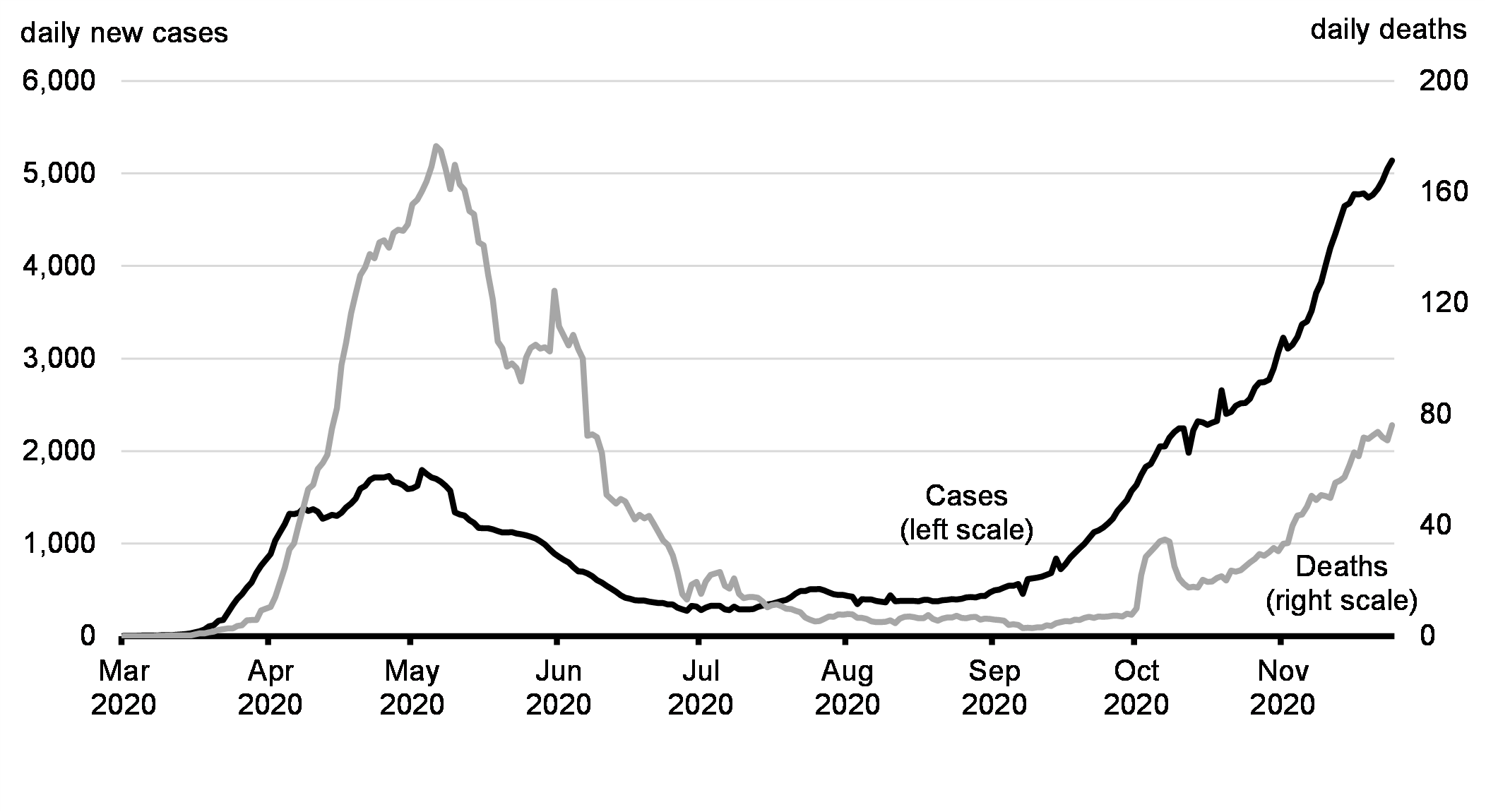
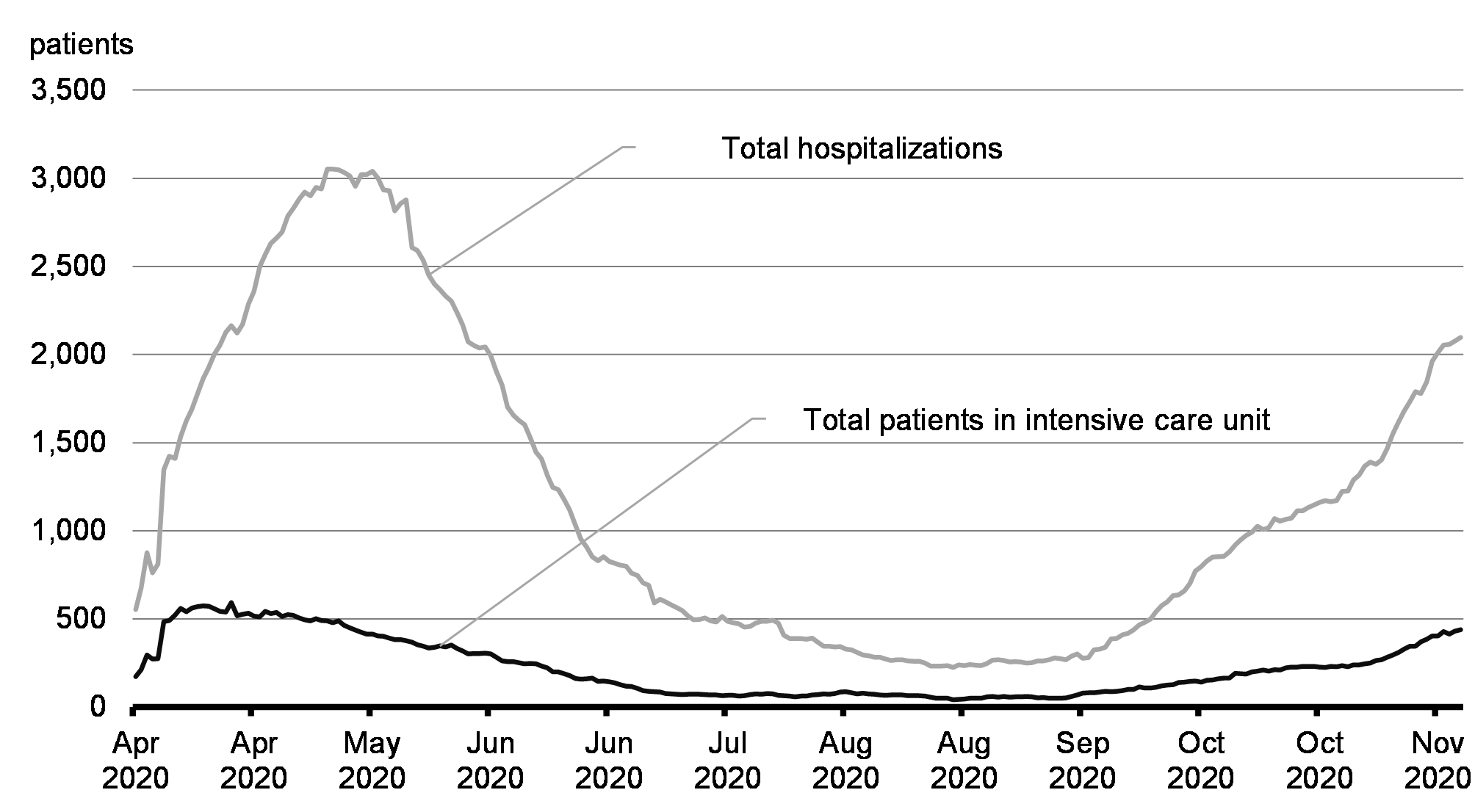
Canada is seeing rapid growth in daily case counts and spread in high risk populations and settings. Of great concern is the fact that deaths and hospitalizations are rising and these figures are expected to rise further if we do not immediately reduce our contacts and follow strong public health measures (Chart 1.2).
Patients in Hospital with COVID-19
1.1.2 International Comparison
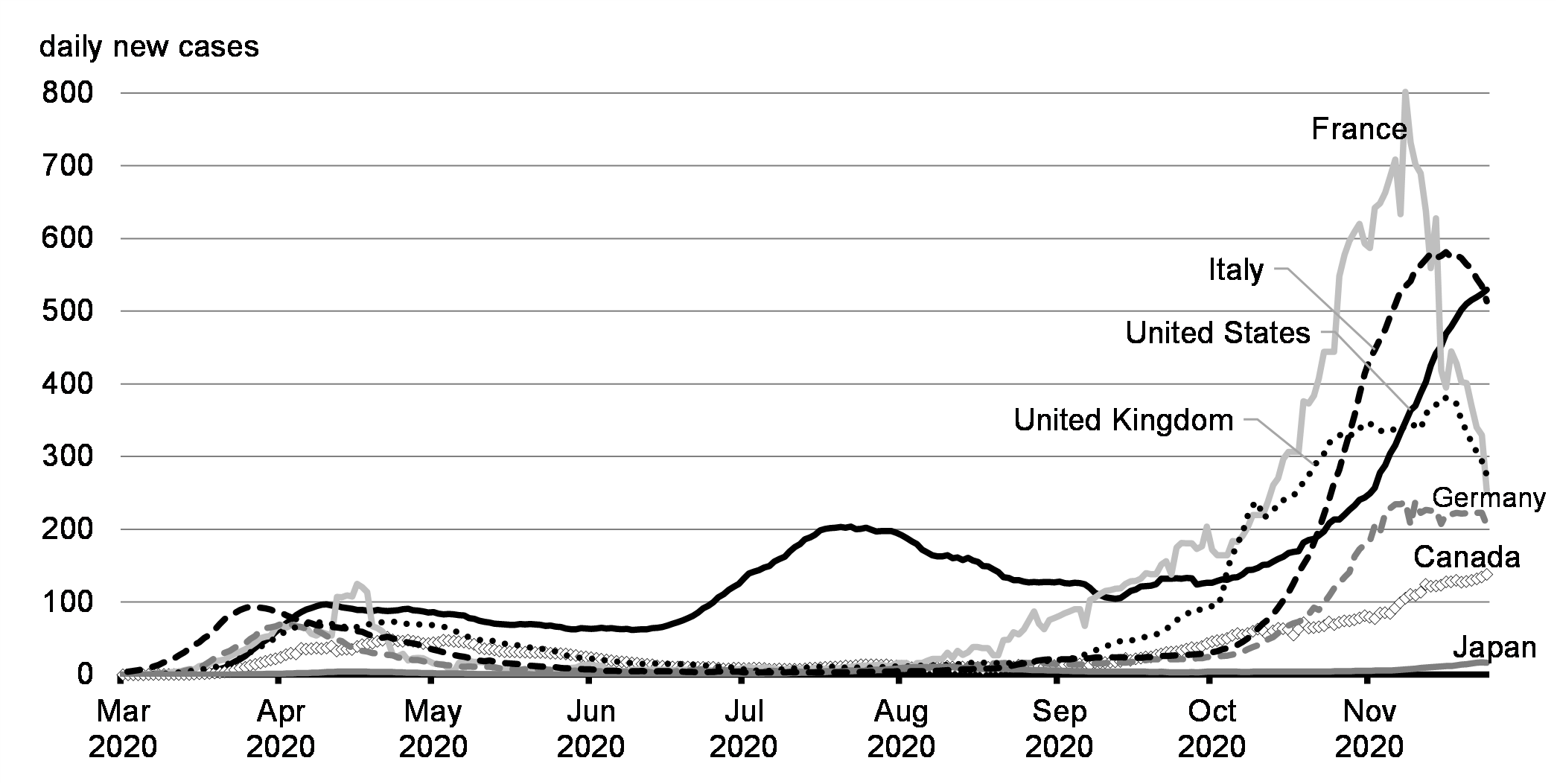
Canada experienced a lower peak of new infections in the first wave than any G7 partners, aside from Japan, and, at present, has the second lowest rate of new infections in the second wave (Chart 1.3). However, recent case increases are concerning. Europe has seen a dramatic spike in infections during its second wave although recent European measures to control the virus appear to be working. Despite Canada neighbouring a country with a very high infection rate, management of the border has limited the spread of COVID-19.
New Cases of COVID-19 per Million People (7-day moving average)
1.1.3 Disproportionate Impacts on Vulnerable Canadians
While there have been strides made in treating the disease, all Canadians must continue to take precautions to prevent the spread. Tragically, COVID-19 is having the worst impact on our most vulnerable and those already facing greater health inequities. Indigenous peoples are at increased risk. Our elders have suffered the most severe cases and face the highest mortality rate. And, recent data from Toronto Public Health shows that people with lower income levels and racialized communities experience higher rates of both contracting and being hospitalized for COVID-19. Another report found that, in Toronto, Black, Latin American, Arab, Middle Eastern or West Asian people are at least seven times more likely to contract COVID-19 than non-racialized people in the city. Across Canada, Statistics Canada data shows that communities with the highest numbers of racialized Canadians had the highest mortality rates during the first wave of the pandemic.
1.2 Supporting a Strong COVID-19 Response
The best economic policy is a strong health policy. The federal government has acted quickly and decisively to support Canadians through this crisis and to help Canadian workers, businesses, provinces, territories, municipalities, Indigenous communities and public health officers to do the right thing.
That is why, since day one, the federal government has made major investments in health care, in procuring medical and personal protective equipment, in income support and paid sick leave, in responding to businesses’ urgent needs, and overall, in keeping Canadians safe, healthy, and solvent through the turbulence of the COVID-19 pandemic.
With the country now in the second wave of the pandemic, the government continues to build on the groundwork it has already laid.
| Federal | Provincial and Territorial |
Total | |
|---|---|---|---|
| Impact ($ billions) | |||
| Direct Measures to Fight COVID-19 and Support People | 322.3 | 60.1 | 382.4 |
| Tax Payment Deferrals | 85.1 | 39.4 | 124.5 |
| Credit Support | 83.4 | 3.3 | 86.7 |
| Total | 490.7 | 102.8 | 593.5 |
| Share of Spending (per cent) | |||
| Direct Measures to Fight COVID-19 and Support People | 84.3 | 15.7 | 100 |
| Tax Payment Deferrals | 68.3 | 31.7 | 100 |
| Credit Support | 96.2 | 3.8 | 100 |
| Total | 82.7 | 17.3 | 100 |
| Notes: Provincial and territorial government announcements; Department of Finance Canada calculations. As of November 13, 2020. For federal totals, the data reflects the total impact which differs from fiscal cost on an accrual basis. Totals may not add due to rounding. | |||
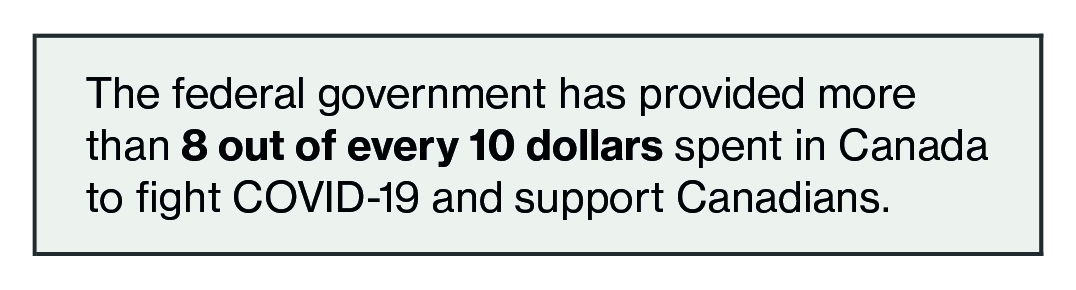
1.3 A Team Canada Approach
Collaboration between different orders of government has been a keystone of Canada’s approach to this global pandemic. The Government of Canada has worked with provinces, territories, municipalities, and Indigenous communities to ensure Canadians stay safe and healthy and have the support they need. To date, the government has invested $322 billion to support Canadians and fight COVID-19. $52 billion of this funding has supported coordinated action to strengthen critical health care systems, purchase personal protective equipment and supplies, and support critical medical research and vaccine development.
1.3.1 A Coordinated Federal-Provincial-Territorial Response
From the beginning, protecting Canadians has been a Team Canada effort. Through measures announced prior to the Fall Economic Statement, direct support made available to provinces and territories totals over $24 billion. The federal government invested to support the capacity of provinces and territories to get the virus under control in their jurisdictions.
“Fighting COVID-19 and safely restarting our economy requires a Team Canada approach. We will continue to work together with provinces and territories to keep Canadians safe and healthy, and to build a more resilient Canada.”
In March, the federal government provided an initial $500 million to provinces and territories to address critical health system needs. Following this immediate support, the Safe Restart Agreement invested $19.9 billion to help provinces and territories safely restart their economies and make Canada more resilient to further waves of the virus, including increased capacity for testing and tracing. Building on the Safe Restart Agreement, the federal government is also providing up to $2 billion under the Safe Return to Class Fund for provinces and territories to support a safe return to class and to protect students and staff.
Federal government support includes the COVID-19 Essential Workers Support Fund, through which the government is providing up to $3 billion to cost-share temporary wage increases for essential workers across the country who have been on the front lines throughout the pandemic.
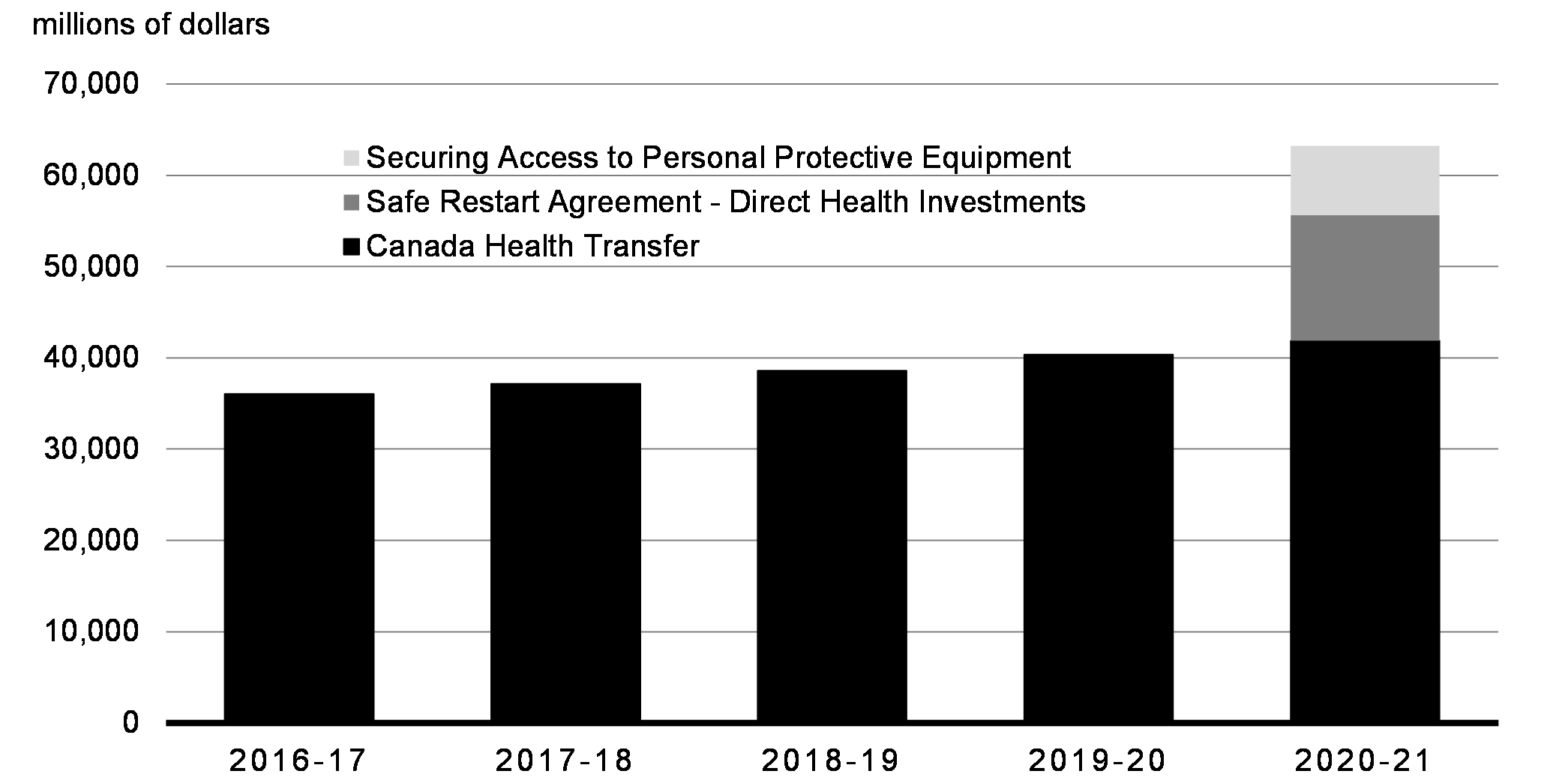
The scope of federal direct support to each province and territory to maintain resilient health care systems has been unprecedented. As a result of the Safe Restart Agreement alone, federal health support for provinces and territories is up by over 23 per cent relative to the previous fiscal year’s Canada Health Transfer.
Federal Investments in Health Care Support
1.3.2 Safe Restart Agreement
This agreement, as adopted by Canada’s First Ministers, was designed to deal with the most pressing issues facing Canadians’ health and safety.It focused on increasing testing and contact tracing capacity across provinces and territories. Funding supported the capacity of our health care systems, including services for people facing mental health challenges. It has also assisted with the procurement of personal protective equipment to help our essential workers, and protect the most vulnerable, like seniors. This agreement was also designed to provide municipalities with much needed funding to support the frontline services they deliver to Canadians.
| Priority Stream | Objectives | Federal Support ($) | |
|---|---|---|---|
| 1 | Testing and contact tracing | Increasing testing capacity to 200,000 tests per day | $4.3 billion |
| Partnering of federal, provincial and territorial governments on the procurement of testing supplies and equipment | |||
| Helping provinces and territories scale up contact tracing capacity | |||
| Contributing to improved data management to share disaggregated data | |||
| 2 | Health care capacity | Helping provinces and territories prepare health care systems for a second wave of COVID-19 Supporting people experiencing mental health and problematic substance use challenges |
$1.2 billion |
| 3 | Personal protective equipment (PPE) | Ensuring health and non-health workers have access to the PPE that they need. This includes $4.5 billion to purchase PPE for national use and $3 billion for provinces and territories for PPE investments. | $7.5 billion |
| 4 | Vulnerable populations | Addressing immediate needs and gaps in supportive care (e.g. home care, long-term care and palliative care) | $740 million |
| Providing health and social supports for other vulnerable groups | |||
| 5 | Child care | Ensuring that a safe, sufficient and adequate supply of child care is available to support the gradual return to work of parents | $625 million |
| Supporting the needs of staff, including through training, extra salary costs and proper equipment (including PPE) to keep children and staff safe | |||
| 6 | Sick leave | This funding announced under the Safe Restart Agreement has been used towards the Canada Recovery Sickness Benefit, which provides income support for workers who are unable to work for reasons related to COVID-19, including those with underlying health conditions | $1.1 billion |
| 7 | Municipalities | Supporting municipalities through COVID-19, including the increasing costs of services and operations | $2 billion |
| 8 | Transit | Providing opt-in matching funding to ensure critical transit services are maintained to support a safe return to work | $2.4 billion |
| TOTAL | $19.9 billion | ||
1.3.3 Supporting a Safe Return to Class
The COVID-19 pandemic has been difficult for families, with schools closed in the spring and students separated from their classmates and friends. The return of Canadian children to school has seen COVID-19 transmission remaining low in school and child care settings. This is due, in no small part, to the tremendous efforts of teachers, administrators, cleaning staff and the many education workers across Canada. For their part, Canada’s children have been remarkable – adapting to the constraints of going to school in the time of COVID-19.
The Safe Return to Class Fund provides the complementary funding provinces and territories need as they work alongside local school boards to ensure the safety of students and staff members throughout the school year. For example, the fund is supporting adapted learning spaces, improved air ventilation, increased hand sanitation and hygiene and the purchase of personal protective equipment and cleaning supplies.
The federal government is providing up to $2 billion to provinces and territories through the Safe Return to Class Fund, building on the Safe Restart Agreement. Already, this fund has helped schools make necessary adaptations and preparations. As a result of the government’s support, employment in the education sector is higher than it was before the pandemic, providing the staffing necessary to keep schools open safely during these challenging times.
Gender Results Framework
Gender Equality and Diversity in Canada
-

Economic Participation and Prosperity
In February 2020, women accounted for 75 per cent of employment in elementary and secondary schools that were suddenly closed and have since re-opened during the pandemic. According to the 2016 Census, visible minorities were underrepresented in elementary and secondary schools relative to their share of all wage earners (12 per cent versus 21 per cent). Immigrants were also underrepresented (15 per cent) compared to their overall employment share (24 per cent).
1.3.4 Support for Indigenous and Northern Communities
Indigenous communities have worked diligently to control the spread of the virus in their communities. The government recognizes that Indigenous and northern communities face unique challenges in responding to the pandemic, including a higher incidence of pre-existing health vulnerabilities, difficulties in accessing healthy food and health services and overcrowded living conditions that make it difficult to physically distance.
Since the launch of the Indigenous Community Support Fund in the spring, the government has provided $685 million to help First Nations, Inuit and Métis communities, as well as Indigenous communities and organizations serving Indigenous peoples, to provide a wide variety of support. These include programs that help elders and vulnerable community members, address food insecurity and support measures that help prevent the spread of COVID-19. This fund has provided support to Indigenous communities and organizations across the country, including contributing to recent targeted investments of over $180 million to Indigenous communities and organizations in Manitoba, Alberta and Saskatchewan to address acute needs during the second wave.
- Building on these investments, the government is proposing to provide a further $380 million in 2020-21 for the Indigenous Community Support Fund to help ensure that the needs of Indigenous communities will continue to be met during the second wave, bringing total investments towards the fund to over $1 billion since the beginning of the pandemic.
To support northern communities and businesses, the government has provided over $272 million, including funding to bolster territorial pandemic preparedness and response, to support northern air carriers and businesses and to help ensure that families living in northern communities can continue to afford nutritious food and hygiene products.
The Government of Canada has committed an additional $112 million for First Nations to support a safe return to schools on reserve and $206.1 million to support a safe restart in Indigenous communities, including adapting community infrastructure and other supports for safe restart in Indigenous post-secondary education institutions and Indigenous early learning and child care.
Building on these investments, the government is proposing to continue to work with First Nations, Inuit, Métis and territorial leaders to ensure that they have the tools they need to keep their communities safe and prevent outbreaks of COVID-19:
- $64.7 million in 2020-21 in direct support to the governments of Yukon, Northwest Territories and Nunavut in further support of territorial COVID-19 pandemic response; and,
- $332.8 million in 2021-22 to support First Nations, Inuit and Métis communities to offset declines in own-source revenues and to help ensure that Indigenous communities can continue to provide the same level of core community programs and services to their members.
1.4 Protecting the Health and Safety of Canadians
1.4.1 Vaccines and Therapeutics
To date, Canada has invested over $1 billion in vaccine agreements and secured a domestic supply of up to 429 million doses of seven promising COVID-19 vaccine candidates. Canada has secured the most diverse portfolio of any country. All Canadians can rest assured that a safe and effective vaccine will be available to them – for free – once it is ready.
Confirmed Vaccine Doses Procured per Person by Vaccine Candidate
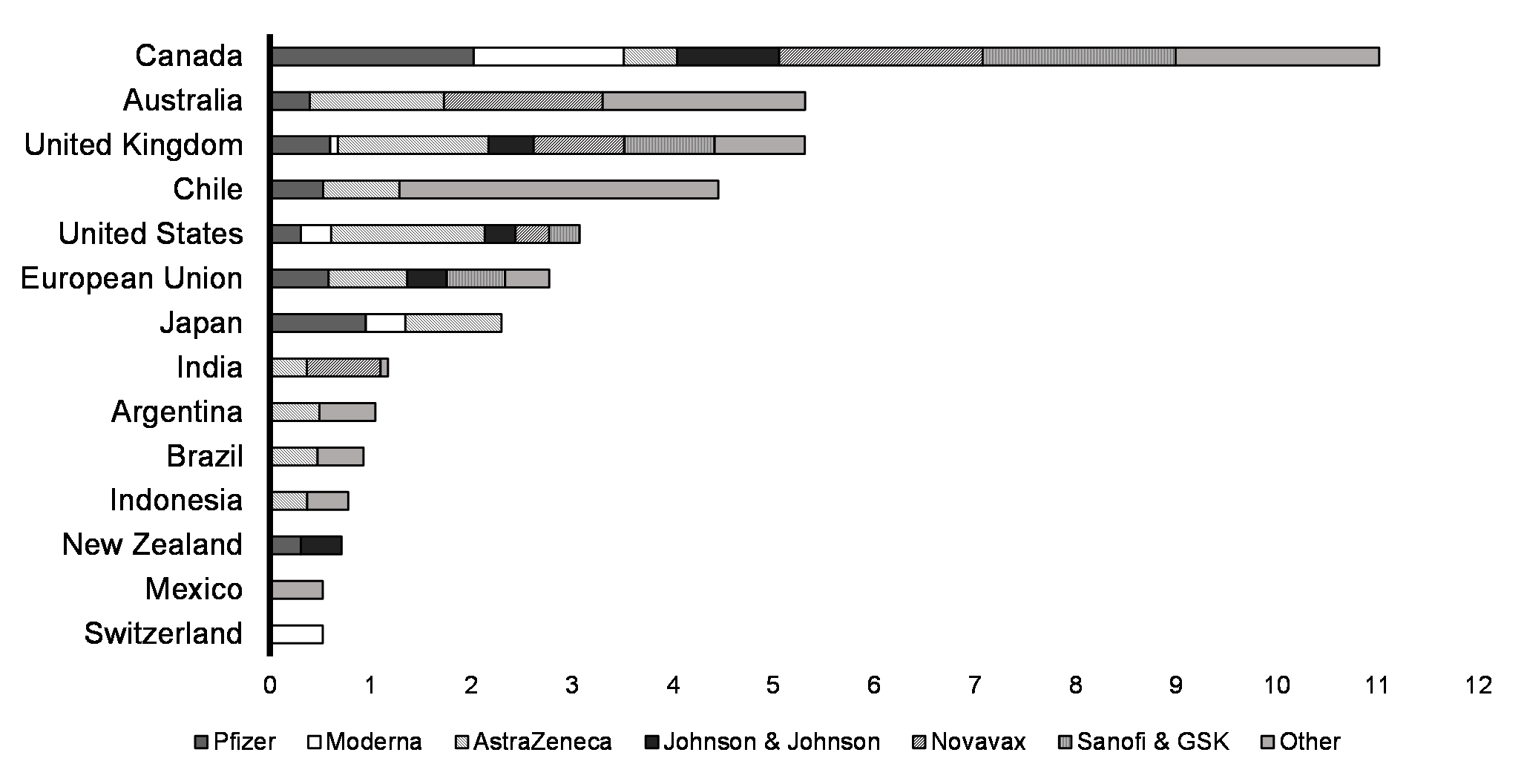
The government is working closely with health officials, provinces, territories and Indigenous partners on key aspects of Canada’s response to the pandemic, including research and development, procurement, bio-manufacturing and distribution of a vaccine. These efforts are supported by experts within the COVID-19 Vaccine Task Force, Therapeutics Task Force and Immunity Task Force.
| Vaccine | Type of Vaccine | Number of Doses |
|---|---|---|
| Pfizer | mRNA | Up to 76 million |
| Moderna | mRNA | Up to 56 million |
| Medicago | Virus-like particle | Up to 76 million |
| AstraZeneca | Viral vector | Up to 20 million |
| Johnson & Johnson | Viral vector | Up to 38 million |
| Novavax | Protein subunit | Up to 76 million |
| Sanofi and GlaxoSmithKline | Protein subunit | Up to 72 million |
| International COVAX Facility | - | Up to 15 million |
1.4.1.1 Investing in Made-in-Canada Vaccine Technologies
The government is investing in ways to enhance Canada’s capacity to discover, manufacture and distribute vaccines, including:
- Investing $126 million in the government’s capacity to manufacture vaccines by establishing a new bio-manufacturing facility at the National Research Council’s Human Health Therapeutics Research Centre in Montréal. This builds on the $44 million already invested in the facility since the onset of COVID-19 and will enable the National Research Council to increase vaccine manufacturing to up to two million doses per month.
- Investing in bio-manufacturing capacity in Canada’s private sector, including at AbCellera and Medicago. These investments are funded through the Strategic Innovation Fund, which has been provided up to $792 million to support, among other things, research and development, clinical trials and manufacturing of vaccines and therapeutics to fight COVID-19.
- Helping Canadian industry to develop a COVID-19 vaccine and therapeutics by providing $23 million to the National Research Council to provide support for research and development.
- Securing equipment and supplies for packaging vaccines once they are manufactured through a $150 million investment in 2020-21.
The government is further committed to ensuring that Canada is well-positioned to respond to future health emergencies and is exploring ways in which it can help promote long-term sustainable growth in Canada’s bio-manufacturing sector. Work is underway to assess current and ongoing needs in the sector and to find ways to complement recent government investments – such as those in the National Research Council’s Montréal facility and via the Strategic Innovation Fund. The Department of Innovation, Science and Economic Development and partner departments will actively engage with stakeholders to explore ways that the government can support future pandemic preparedness, including vaccine manufacturing in Canada.
Gender Results Framework
Gender Equality and Diversity in Canada
-

Economic Participation and Prosperity
In October 2020, women represented 57 per cent of biologists and related scientists, which includes such occupations such as virologist, microbiologist, and immunologist, among others. Women also represented 61 per cent of biological technologists and technicians, up from 51 per cent in February 2020, reflecting strong employment growth in this occupation, likely related to testing activity.
1.4.1.2 Vaccination Roll-out Preparedness
Since May, in preparation for vaccine roll-out, the government has invested a total of $284.2 million to improve our capacity to distribute COVID-19 vaccines to Canadians. This investment includes $125 million in 2020-21 for the shipping and storage of COVID-19 vaccines and $159.2 million, starting in 2020-21, to procure supplies needed to vaccinate Canadians (e.g. needles, alcohol swabs) and increase vaccine deployment capacity through improved infrastructure, promotion and national guidelines for the delivery of vaccines.
Rolling out vaccines will be a complex national endeavour. As part of continuing preparations for the distribution of a vaccine, Canada is working with provinces, territories, Indigenous partners and private sector partners to ensure the appropriate planning and infrastructure is in place to receive and deploy vaccines. Canada is supporting a coordinated approach, including through joint development of plans with provinces and territories, and by providing nationwide logistical support and warehousing services to supplement provincial and territorial capacity. In addition, Canada is securing specialized freezer capacity to hold tens of millions of doses at any given time, ensuring we can handle the specifications of potential vaccine candidates. This Team Canada approach will ensure that everyone can access a COVID-19 vaccine as seamlessly as possible, including in remote and isolated communities. The Canadian Armed Forces are working with the Public Health Agency of Canada to assist in logistics planning for the rollout of COVID-19 vaccines.
Just like Canada’s COVID-19 response, regulatory approval of a vaccine will be informed by science. Canada has invested in Health Canada to ensure its scientists can prioritize the review of COVID-19 vaccines, and work has begun – Canada is currently reviewing three vaccine submissions. The government has put in place an agile process that allows for review on a rolling basis. This will ensure promising vaccine candidates receive timely review and are approved when found to be safe and effective. Once our scientists approve a vaccine, the federal government, provinces and territories will be ready to ensure Canadians can access the vaccine in a timely manner, including accelerated access to priority populations, such as those most vulnerable to COVID-19.
1.4.2 Testing and Contact Tracing
The Government of Canada has made significant investments to ensure Canadians can be tested for COVID-19. This included seeking a commitment from provinces and territories to increase testing capacity to up to 200,000 tests per day and providing $4.28 billion to help them reach that goal. This support is also there so provinces and territories can conduct contact tracing and improve data on COVID-19. The COVID Alert smartphone application is facilitating contact tracing through anonymous exposure notifications. Hundreds of federal government employees are also helping provinces with contact tracing, at no cost. The federal government has agreements in place with seven provinces – New Brunswick, Quebec, Ontario, Manitoba, Saskatchewan, Alberta, and British Columbia – for federal government employees to provide assistance with contact tracing. Federal government employees can make nearly 18,000 contact tracing calls per day.
The percentage of tests coming back positive has risen recently and, as of mid-November, is above 7 per cent, on average, nationally. The higher the percentage, the higher the potential for transmission and the greater the likelihood that there are undetected cases of COVID-19 in the community. Continuing to ramp up testing and tracing is critical to detecting and isolating infections and ultimately reducing the spread of the virus.
1.4.2.1 Scaling Up Testing Capacity
The government has made substantial investments to ensure Canada is prepared for subsequent waves of COVID-19. This includes an enhancement of 6,000 tests per day within Canada’s National Microbiology Laboratory to support the provinces and territories in their testing efforts. It also includes continued monitoring of the risk of transmission in the community in order to support outbreak management and infection prevention and control.
- To support Canada’s continued COVID-19 response, the government proposes to provide $565.4 million to Health Canada and the Public Health Agency of Canada to ensure that federal and provincial laboratories continue to receive sufficient testing supplies and to support the roll-out of new rapid COVID-19 tests and innovative approaches to testing. $37.4 million of this proposed funding will support research, development, and modelling initiatives to track and identify the spread of the virus. For example, new science has demonstrated that monitoring COVID-19 in wastewater can serve as a critical surveillance tool for early detection and intervention in communities. Investing in wastewater analysis research has the potential to complement conventional COVID-19 testing and screening measures by identifying community spread early.
1.4.2.2 Rapid Testing
With rising COVID-19 cases, quick and accurate testing has become more important than ever. The government has been working to secure rapid testing technology. These new rapid tests can be analyzed on-the-spot, with results available in minutes. The procurement and deployment of these tests will aid in meeting the urgent demands from provinces and territories to test more Canadians, more frequently and reduce wait times for results, including in rural and remote communities without a laboratory nearby.
The government is working to review, approve, purchase and deploy COVID-19 rapid tests as quickly as possible.
| Company | Test Name | Number of Tests |
|---|---|---|
| Abbott Rapid Diagnostics | ID NOW | Up to 7.9 million |
| Abbott Rapid Diagnostics | Panbio | Up to 20.5 million |
| BD | BD Veritor | Up to 7.6 million |
| bioMérieux Canada | BIOFIRE RP2.1 | Up to 700 thousand |
| Inter Medico | Cepheid GeneXpert | Up to 1.2 million |
To date, more than 5 million rapid test kits have been delivered to provinces and territories. In total, Canada signed agreements for up to 38 million rapid tests which is over three times the total number of tests performed to date. This includes rapid tests that were deployed to remote communities earlier in the pandemic.
COVID Alert App

Canada’s COVID-19 exposure notification app is a nationwide mobile app that lets users know if they have been exposed to COVID-19. The app is available to all Canadians and is currently connected to the health systems in Northwest Territories and every province except British Columbia and Alberta.
The app notifies users of potential exposure to the virus so they can take necessary precautions, get tested and know to monitor for symptoms. No matter where in the country someone lives, the app still notifies users of a possible COVID-19 exposure from someone in a jurisdiction where the app is fully on-line.
The app protects users’ privacy and does not track users’ location or collect identifiable information. As of late-November, there have been more than 5.5 million downloads of the app and over 6,200 positive cases registered using the app, notifying untold thousands more people of a potential exposure and preventing thousands more new cases.
- The government proposes to provide $20.5 million in funding to the Canadian Digital Service to continue delivering existing critical services, including the COVID Alert App, and to recruit talent that meets the demands for digital services stemming from COVID-19 and other government priorities. .
1.4.3 PPE and Medical Equipment
The federal government has committed over $7.6 billion to rapidly procure more than two billion pieces of personal protective equipment. Canada continues to aggressively procure vital supplies to keep our nurses, doctors and frontline health care workers well-equipped and to keep all Canadians safe in the months and years ahead. This funding is in addition to the $3 billion for PPE procurement provided directly to provinces and territories through the Safe Restart Agreement.
The bulk of federally procured PPE and medical supplies is provided to provinces, territories and Indigenous communities, while a portion is retained for federal usage or held in reserve as part of the National Emergency Strategic Stockpile (NESS).
- The Government of Canada is also allocating an additional $1.5 billion, on top of prior amounts, in order to continue to procure PPE and provide warehousing and logistics support to rapidly deliver critical PPE and medical supplies to provinces, territories and Indigenous communities, as well as to maintain the readiness of the NESS.
Gender Results Framework
Gender Equality and Diversity in Canada
-

Economic Participation and Prosperity
Women are overrepresented in many frontline settings, including hospitals and long-term care homes. The greater risk of transmission of COVID-19 that this entails also means that investments in PPE triggered by the pandemic will disproportionately benefit women. In 2019, women comprised 91 per cent of registered nurses, 92 per cent of nurse practitioners and 91 per cent of licensed practical nurses. Immigrants and visible minorities are also overrepresented in certain frontline occupations. In 2016, more than one-third of nurse aides, orderlies and patient service associates were immigrants (86 per cent of which were women) compared to one-quarter of all other occupations. They were also more likely to identify as a visible minority (34 per cent) than workers in other occupations (21 per cent), with Black and Filipino women especially overrepresented.
As community transmission has re-emerged in Canada, public health officials in Canada are emphasizing the importance of maintaining physical distancing in public places and using face masks to help curtail the spread of COVID-19.
- To support these public health measures and help keep Canadians safe, the government is proposing to remove the Goods and Services Tax/Harmonized Sales Tax (GST/HST) from the purchases of face masks and face shields. This will make these important items more affordable. This would provide $75 million annually in tax relief to Canadians and be effective from December 7, 2020, until the use of face coverings is no longer broadly recommended.
1.4.3.1 Made-in-Canada Approach
Since the government’s call to action on March 20, 2020, for Canadian industry to support the country’s response to the COVID-19 pandemic, over 6,500 companies, organizations, and individual Canadians have stepped forward to offer their expertise and assistance. To date this initiative has successfully secured domestic production for a range of critical PPE, medical devices and associated commodities. This includes surgical masks, medical gowns, face shields, ventilators and testing components.
The government also moved quickly to ensure there would be a reliable, Canadian-made supply of N95 masks by entering into a long-term purchase agreement with Medicom, located in Montréal. At least three million made-in-Canada masks have already been delivered. In partnership with the Government of Ontario, the government also invested in a 3M facility in Brockville, Ontario, that will begin delivering Canadian-made N95 masks in 2021.
1.4.4 Ensuring Clean and Healthy Ventilation in Public Buildings
Guidance from public health authorities indicates that the risk of COVID-19 transmission can be higher in closed spaces with poor ventilation.
- Building on investments made through the COVID-19 Resilience Stream under the Investing in Canada Infrastructure Program and the Safe Return to Class Fund, the government proposes to provide $150 million over three years, starting in 2020-21, to Infrastructure Canada to improve ventilation in public buildings and help reduce the spread of COVID-19. This will help provincial, territorial, municipal and local governments and Indigenous communities fund projects that increase air quality and circulation, such as upgrades or conversions of heating, ventilation and air conditioning systems. More details on this measure will be announced in the coming months.
1.4.5 Preventing Outbreaks in Shelters
The COVID-19 pandemic has placed significant new funding pressures on Canada’s shelters that, in order to prevent outbreaks among people, have had to transform how they deliver services.
- To enable physical distancing, enhanced cleaning and other emergency health and safety measures to prevent the spread of COVID-19 in shelters, the government will provide additional funding of $299.4 million in 2021-22 through Reaching Home: Canada’s Homelessness Strategy. Funding will also help prevent at-risk Canadians from becoming homeless by supporting targeted interventions that enable people to stay housed.
This is in addition to the government’s September 2020 announcement of $236.7 million to extend support for community-led responses to COVID-19 through Reaching Home. This builds on the $157.5 million announced in the spring, which enabled emergency shelters to implement physical distancing and other measures to protect health and safety.
1.4.6 Border Measures
To help control the spread of COVID-19 in Canada, the government has also put in place restrictions and protective measures at its borders:
- In March, Canada and the United States mutually agreed to temporarily restrict all non-essential travel across the Canada-U.S. border to protect people on both sides of the border while ensuring the flow of essential goods and services.
- All travellers entering Canada, whether or not they are Canadian citizens, are subject to a mandatory quarantine.
- The government has also enhanced the presence of public health officials at key points of entry. To manage risks, international travellers continue to be screened for symptoms of COVID-19 prior to entering the country.
1.4.7 Quarantine and Self-isolation Support
Canada is providing resources so that people who need to quarantine or self-isolate have a place to go.
- To ensure all arriving travellers follow quarantine orders, the government provided $322 million in 2020-21 to maintain quarantine facilities at Canada’s four largest airports and other locations in Canada for greater national coverage.
- In addition, to support vulnerable persons who cannot safely or effectively self-isolate upon a confirmed or suspected case of COVID-19 (e.g. crowded housing), the government has invested $100 million over two years, starting in 2020-21, to support safe voluntary isolation sites in municipalities across Canada.
- To support employers in the farming, fish harvesting and food processing sectors who are facing extraordinary costs associated with ensuring temporary foreign workers isolate for 14 days, as required under the Quarantine Act, the government provided $54 million in 2020-21 to offset costs.
- The government proposes to provide up to an additional $34.4 million in 2020-21 to continue the Mandatory Isolation Support for Temporary Foreign Workers Program, which will extend this support to the end of March 2021.
1.5 Long-term Care
The devastating COVID-19 outbreaks in long-term care homes have highlighted the gaps in standards and care for our most vulnerable. A large majority of COVID-19 deaths have occurred in long-term care facilities and seniors residences. In Quebec and Ontario these have been 81 per cent and 70 per cent of fatalities, respectively, as of November 25.
From April to July 2020, Operation Laser deployed women and men of the Canadian Armed Forces (CAF) to support 54 affected long-term care facilities across Quebec and Ontario. At peak response, 1,942 CAF personnel were helping care for residents.
Many personal support workers continue to bravely go to work and provide essential care to vulnerable seniors, despite the threat of infection.
Gender Results Framework
Gender Equality and Diversity in Canada
-

Poverty Reduction, Health and Well-Being
-

Economic Participation and Prosperity
The pandemic has highlighted the gendered nature of long-term care in Canada. According to the 2016 Census, men accounted for 60 per cent of residents in residential care facilities for persons with disabilities and addictions, but women accounted for 69 per cent of all residents in nursing homes and residences for senior citizens. Women also accounted for the largest share of staff in long-term care facilities. In particular, in February 2020, according to the Labour Force Survey, women accounted for 82 per cent of employment in nursing and residential care facilities and 82 per cent of employment in home health care services. Two other groups – immigrants and visible minorities – were also overrepresented in nursing and residential care facilities and home health care services according to the 2016 Census.
1.5.1 Helping Provinces and Territories Protect Long-term Care and Other Supportive Care Facilities
Seniors deserve to be safe, respected and live in dignity. Through the Safe Restart Agreement, the federal government invested $740 million to help provinces and territories address immediate needs of vulnerable populations, including those in long-term care. The federal government has helped provinces and territories to fight the outbreaks in long-term care facilities by providing PPE, contact tracing and over $39 million in funding for direct assistance through the Canadian Red Cross.
From day one, the federal government has worked with the provinces and territories to protect the most vulnerable, including supporting Canadian Red Cross work in a number of long-term care facilities. In Manitoba, which has been hit hard in the second wave, the federal government has approved a request for support in their long-term care facilities until January 15, 2021.
- In addition to these efforts and building on what we have learned from the CAF deployment in long-term care homes, the Government of Canada is committing up to $1 billion for a Safe Long-term Care Fund, to help provinces and territories protect people in long-term care and support infection prevention and control. Funding will be contingent on a detailed spending plan, allocated on an equal per capita basis and conditional on provinces and territories demonstrating that investments have been made according to those spending plans. Provinces and territories will be able to use this funding to undertake a range of activities, including carrying out infection prevention and control readiness assessments, making improvements to ventilation and hiring additional staff or topping up wages.
- Further, the government is committing $6.4 million over two years, starting in 2020-21, to the Canadian Foundation for Health Improvement to expand its LTC+ initiative, which allows long-term care facilities and seniors residences to register via an online portal and submit a self-assessment, making them eligible for coaching and seed funding to help address gaps. The additional funding is expected to allow LTC+ to expand its reach to about 1,000 facilities across Canada.
- The government is also committing $1 million to engage with third parties to help identify resources to conduct readiness assessments in long-term care facilities and facilitate training on infection prevention and control.
- Furthermore, the government is committing $2.4 million over three years to expand Health Canada’s capacity to support these new initiatives and undertake policy work related to commitments made in the Speech from the Throne.
Additionally, in cooperation with provinces and territories, the federal government provided substantial support to give essential workers a raise, including personal support workers and other frontline workers. In addition, the government is also committing $38.5 million over two years to support training up to 4,000 personal support worker interns through an accelerated 6-week online training program combined with a 4-month work placement, to address acute labour shortages in long-term care and home care.
One in four of the workers in our health sector are immigrants. They have been on the front lines of this pandemic, helping care for all Canadians, particularly those in long-term care. Many asylum seekers are among this group. In recognition of these “Guardian Angels” – asylum claimants working in the health care sector during the COVID-19 pandemic – playing a critical role in keeping Canadians healthy, the government announced a temporary measure that will provide a pathway to permanent residency for them.
1.5.2 New National Standards
In order to make sure seniors and those in care live in safe and dignified conditions, the federal government will work with provinces and territories to set new, national standards for long-term care. The government remains committed to establishing these standards as a means to address critical gaps in long-term care facilities, including raising the working conditions of lower-wage essential workers in senior care, particularly personal support workers, who have persevered in the face of adversity. Solutions will be explored to improve retention, recruitment and retirement savings options for low- and modest-income workers, as discussed in Chapter 3.
1.6 Helping Vulnerable Canadians and Improving Public Health
1.6.1 Mental Health and Virtual Care
The emotional and mental health effects of the pandemic are likely to be ongoing as we face the second wave and public health measures are in place and economic uncertainty continues. 50 per cent of Canadians report that their mental health has worsened during COVID-19. The Canada Suicide Prevention Service is also reporting a 50 per cent increase in call volume.
The government has invested $500 million through the Safe Restart Agreement to address immediate needs and gaps in the support and protection of people experiencing challenges related to mental health, substance use or homelessness.
The government has also funded the development of virtual mental health care applications and has launched a free online portal, Wellness Together Canada. Site visitors have free access to educational content, self-guided therapy, moderated peer-to-peer support and one-to-one counseling with qualified health professionals. Since April 2020, there have been over 648,000 unique visitors to the Wellness Together Canada portal and 1.8 million sessions (e.g. text or phone interaction with qualified health professionals or peer support networks). Canadians from all provinces and territories have accessed the portal.
- To help Canadians through this difficult time, the government is investing an additional $93 million in 2020-21. This includes $50 million to bolster distress centres and $43 million to provide further support for the Wellness Together Canada portal and the resources it offers.
Gender Results Framework
Gender Equality and Diversity in Canada
-

Poverty Reduction, Health and Well-Being
In a crowdsourcing survey from April 24 to May 11, 2020, 71 per cent of gender diverse participants reported that their mental health is “somewhat worse” or “much worse” since physical distancing began, compared to 57 per cent of female participants and 47 per cent of male participants. Indigenous participants were also more likely to report somewhat or much worse mental health (60 per cent) in this same crowdsourcing survey than non-Indigenous participants (52 per cent). Indigenous women in particular noted this impact more than Indigenous men (64 per cent versus 54 per cent). In a separate crowdsourcing survey on Canadians living with long-term conditions and disabilities, 57 per cent reported experiencing “somewhat worse” or “much worse” mental health since the beginning of the pandemic. Previous research demonstrates that the mental health of younger Canadians has been particularly affected by the pandemic and quarantine.
Note on Methodology
Although crowdsourcing surveys are key in obtaining timely information about important issues, such as the extent to which COVID-19 is affecting the lives and well-being of different groups of Canadians, readers should note that unlike other surveys conducted by Statistics Canada, the lack of probability-based sampling means that the findings are not representative and cannot be applied to the overall Canadian population. In particular, some groups of Canadians may be overrepresented, while other groups may be underrepresented.
1.6.2 Fighting the Opioid Crisis
The opioid crisis has taken far too many lives in Canada. The government has adopted a harm reduction approach which includes funding safe consumption sites.
However, the COVID-19 crisis has coincided with a worsening of the opioid crisis and a surge in opioid deaths. A recent study in Ontario found that over the first 15 weeks of the pandemic, there were 695 opioid-related deaths, a 38 per cent increase over the previous 15 weeks. Similarly, British Columbia has also experienced a large increase in opioid-related deaths and overdoses. In June 2020, 181 British Columbians died due to opioid use, compared to 76 in June 2019. British Columbia paramedics reported nearly 7,500 overdose calls in summer, the highest ever in a three-month stretch. Between April and June there were 302 opioid-related deaths in Alberta, up from 2018’s previously recorded three-month high of 211 deaths.
- To support Canadians struggling with problematic substance use, and building on significant funding provided in Budget 2018 and Budget 2019, the government will provide an additional $66 million over two years, starting in 2020-21, to support community-based organizations responding to substance use issues, including to help them provide frontline services in a COVID-19 context.
1.6.3 Pharmacare
The government is taking concrete steps toward the implementation of national, universal pharmacare.
In 2018, the Government of Canada established the Advisory Council on the Implementation of National Pharmacare to provide independent advice on how to best implement national universal pharmacare. Based on the advice of the Council, the government is working with provinces, territories and other stakeholders to move forward in establishing the foundational elements of national, universal pharmacare, including:
- A new Canadian Drug Agency that would negotiate drug prices on behalf of all Canadians, thereby lowering costs.
- A national formulary to be developed by the Canadian Drug Agency.
- A national strategy for high-cost drugs for rare diseases, with funding of $500 million per year, ongoing, starting in 2022-23.
- In the coming weeks, Health Canada will be setting out options for this strategy and will engage with provinces, territories, patients, industry and other interested groups to confirm the path forward.
Making High-Cost Drugs for Rare Diseases More Accessible
There are more than 7,000 rare diseases and although each one affects a relatively small number of patients, these diseases are life-threatening, debilitating and chronic health conditions. The high cost of many drugs for rare diseases and the limited clinical evidence (often limited because of small patient populations) make it difficult for patients and their families, employers and governments to make decisions on whether and how to pay for treatment. This can lead to challenges for many provinces and territories looking to help families. A national strategy will ensure more effective assessments of a drug's efficacy, better manage costs and, crucially, expand coverage and access for patients.
1.6.4 Supporting the Canadian Red Cross Response to COVID-19
Since the early days of the pandemic, the Canadian Red Cross has made an important contribution to Canada’s response to COVID-19. Currently, the Canadian Red Cross is deployed to over 35 sites across the country with the support of federal funding.
In May 2020, the government announced up to $100 million in funding to help the organization meet increased demand due to COVID-19 while ensuring that it can also respond to other emergencies such as flood and wildfire relief efforts. Through this funding, the Canadian Red Cross has been able to provide surge capacity to provinces and territories and protect vulnerable populations, including residents in long-term care facilities and migrant workers.
- To continue supporting the Canadian Red Cross efforts to respond to COVID-19 and other emergencies, the government proposes to make available an additional $35 million in 2020-21.
The COVID-19 pandemic has demonstrated the importance of having surge capacity readily available. Typically, organizations like the Red Cross are largely dependent on event-specific private and public contributions.
- The government proposes to provide $150 million over two years, starting in 2021-22, to support the Canadian Red Cross and other non-governmental organizations in building and maintaining a humanitarian workforce to provide surge capacity in response to COVID-19 outbreaks and other large-scale emergencies.
1.6.5 Continuing to Support the Health Response in Indigenous Communities
The government swiftly began working in partnership with First Nations, Inuit and Métis leaders to support pandemic preparedness and response in Indigenous communities. While Indigenous communities were successful in controlling the spread of COVID-19 during the spring outbreak, now during the second wave, they are reporting alarming surges in COVID-19 cases.
To help ensure that First Nations, Inuit and Métis Nation communities can manage and control the virus during the second wave, as well as the influenza season, the Government of Canada is proposing to commit over $900 million to support the continued health response in Indigenous communities including:
- $631.6 million over two years, starting in 2020-21, in additional support for the ongoing public health response to COVID-19 in Indigenous communities. This brings the total COVID-19 emergency health funding to $926.7 million.
As previously announced by the Minister of Indigenous Services, $82.5 million in 2020-21 to provide surge capacity to address mental wellness needs in Indigenous communities related to COVID-19 pressures.
- $186.8 million over two years, starting in 2020-21, to address needs and gaps in supportive care facilities and provide additional home care in Indigenous communities, in order to protect elders and other vulnerable community members from COVID-19.
1.7 Contributing on the Global Stage
In a global pandemic, we cannot beat this virus here at home until we beat it everywhere.
Canada is leading international coordination and cooperative efforts to provide equitable access to vaccinations, support global economic stability and help foster an inclusive recovery, including:
- Investing $440 million through the COVAX Advance Market Commitment and COVAX Facility to purchase vaccine doses for low- and middle-income countries while also securing up to 15 million doses for Canadians. Canada’s contribution will help deliver fair, equitable and timely access to COVID-19 vaccines.
- Co-convening, with Jamaica and the United Nations, the Financing for Development in the Era of COVID-19 and Beyond process and providing $400 million in 2020-21 in international development funding to address short-term humanitarian and development needs caused by the pandemic and other crises.
- Working closely with G7 and G20 partners to develop and endorse the G20 Action Plan – Supporting the Global Economy Through the COVID-19 Pandemic and its updates. This Action Plan is promoting international cooperation, continuing financial support for citizens by governments that can afford it and helping to secure a global recovery that addresses the disproportionate impact of the crisis on women, young people, and the most vulnerable segments of the population.
- As part of the Action Plan, G20 and Paris Club countries have provided an estimated US$5.7 billion in temporary debt payment relief to some of the world’s poorest countries through the Debt Service Suspension Initiative. Of this, Canada has provided over $40 million in debt payment relief.
- Extending a new $1 billion loan to the International Monetary Fund’s Poverty Reduction and Growth Trust, which funds interest-free loans to low-income countries.
| COVID-19 Economic Response Plan – Protecting Health and Safety |
Impact Value1 |
Net Fiscal Impact (Accrual) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 2019– 2020 |
2020– 2021 |
2021– 2022 |
2022– 2023 |
2023– 2024 |
2024– 2025 |
2025– 2026 |
Included or Announced: | ||
| 1.3.2 Safe Restart Agreement | 19,909 | - | 19,909 | - | - | - | - | - | Policy Action Announced since the July 2020 Snapshot |
| Safe Restart Agreement – | |||||||||
Amount announced in 2020 Snapshot |
14,000 | - | 14,000 | - | - | - | - | - | Policy Action Included in the July 2020 Snapshot |
Further investments since 2020 Snapshot |
3,527 | - | 3,527 | - | - | - | - | - | Policy Action Announced since the July 2020 Snapshot |
Federal Investments in Testing, Contact Tracing, and Data Management |
1,282 | - | 1,282 | - | - | - | - | - | Policy Action Announced since the July 2020 Snapshot |
Sick leave (towards the Canada Recovery Sickness Benefit) |
1,100 | - | 1,100 | - | - | - | - | - | Policy Action Announced since the July 2020 Snapshot |
| 1.3.3 Supporting a Safe Return to Class | 2,000 | - | 2,000 | - | - | - | - | - | Policy Action Announced since the July 2020 Snapshot |
| Safe Return to Class Fund | 2,000 | - | 2,000 | - | - | - | - | - | Policy Action Announced since the July 2020 Snapshot |
| 1.3.4 Support for Indigenous and Northern Communities | 2,069 | - | 1,679 | 391 | - | - | - | - | Policy Action Announced since the July 2020 Snapshot |
| Health and Social Support for Northern Communities (critical priorities, air carriers, food subsidy enhancement) (2020 Snapshot) | 115 | - | 115 | - | - | - | - | - | Policy Action Included in the July 2020 Snapshot |
| Support for Essential Air Access to Remote Communities | 174 | - | 116 | 58 | - | - | - | - | Policy Action Announced since the July 2020 Snapshot |
| Indigenous Community Support Fund – | Policy Action Announced since the July 2020 Snapshot | ||||||||
Amount in 2020 Snapshot |
380 | - | 380 | - | - | - | - | - | Policy Action Included in the July 2020 Snapshot |
Further support announced in August 2020 |
305 | - | 305 | - | - | - | - | - | Policy Action Announced since the July 2020 Snapshot |
Additional support announced in this Statement |
380 | - | 380 | - | - | - | - | - | New in this Fall Economic Statement |
| Safe Restart Framework for Indigenous Communities | 318 | - | 318 | - | - | - | - | - | Policy Action Announced since the July 2020 Snapshot |
| Offsetting declines in Indigenous own-source revenues | 333 | - | - | 333 | - | - | - | - | New in this Fall Economic Statement |
| Direct support to Yukon, Northwest Territories and Nunavut in further support of territorial COVID-19 pandemic response | 65 | - | 65 | - | - | - | - | - | New in this Fall Economic Statement |
| 1.4.1 Vaccines and Therapeutics | 14,340 | - | 7,520 | 6,530 | 340 | 236 | 131 | 119 | |
| Support for Medical Research and Vaccine Developments (2020 Snapshot) | 1,127 | - | 721 | 401 | 8 | 8 | 8 | 8 | Policy Action Included in the July 2020 Snapshot |
| Further Support for medical research and vaccine2 | 13,087 | - | 6,789 | 6,109 | 310 | 205 | 101 | 88 | Policy Action Announced since the July 2020 Snapshot |
| Bio-manufacturing Capacity Expansion – National Research Council Royalmount Facility | 126 | - | 10 | 19 | 23 | 23 | 23 | 23 | Policy Action Announced since the July 2020 Snapshot |
| 1.4.2 Testing and Contact Tracing | 1,370 | 0 | 779 | 569 | 24 | 5 | 5 | 5 | |
| Innovative Research and Support for New Testing Approaches and Technologies | 546 | - | 530 | 16 | 19 | - | - | - | New in this Fall Economic Statement |
| Supporting and Sustaining the Public Health Agency of Canada and Health Canada's Pandemic Operations | 803 | - | 244 | 538 | 5 | 5 | 5 | 5 | New in this Fall Economic Statement |
| Canadian Digital Service | 21 | - | 5 | 15 | - | - | - | - | New in this Fall Economic Statement |
| 1.4.3 PPE and Medical Equipment | 5,352 | 200 | 3,331 | 1,821 | 170 | 113 | 4 | 4 | |
Funding for Personal Protective Equipment and Supplies (Public Health Agency of Canada) (2020 Snapshot) |
2,000 | 200 | 1,800 | - | - | - | - | - | Policy Action Included in the July 2020 Snapshot |
PPE and Related Equipment Support for Essential Workers (funding for procurement) (Public Services and Procurement) (2020 Snapshot) |
11 | - | 11 | - | - | - | - | - | Policy Action Included in the July 2020 Snapshot |
| PPE and Related Equipment Support for Essential Workers (increased support) (Public Services and Procurement) | 500 | - | 500 | - | - | - | - | - | Policy Action Announced since the July 2020 Snapshot |
| Additional PPE Procurement and Support for the Storage and Warehousing of PPE | 2,746 | - | 1,000 | 1,746 | 170 | 113 | 4 | 4 | New in this Fall Economic Statement |
| GST/HST Relief on Face Masks and Face Shields | 95 | - | 20 | 75 | - | - | - | - | New in this Fall Economic Statement |
| 1.4.4 Ensuring Clean and Healthy Ventilation in Public Buildings | 110 | - | 30 | 80 | 40 | - | - | - | |
| Improving Ventilation in Buildings | 110 | - | 30 | 80 | 40 | - | - | Policy Action Announced since the July 2020 Snapshot | |
| 1.4.5 Preventing Outbreaks in Shelters | 694 | - | 394 | 299 | - | - | - | - | |
| Support for the Homeless (through Reaching Home) (2020 Snapshot) | 158 | - | 158 | - | - | - | - | - | Policy Action Included in the July 2020 Snapshot |
| Extended Support For Community-Led Responses to COVID-19 through Reaching Home | 237 | - | 237 | - | - | - | - | - | Policy Action Announced since the July 2020 Snapshot |
| Additional funding through Reaching Home: Canada’s Homelessness Strategy to prevent the spread of COVID-19 in shelters | 299 | - | - | 299 | - | - | - | - | New in this Fall Economic Statement |
| 1.4.7 Quarantine and Self-Isolation Support | 908 | - | 650 | 256 | - | - | - | - | |
| Quarantine Facilities and COVID-19 Border Measures | 765 | - | 507 | 256 | - | - | - | - | Policy Action Announced since the July 2020 Snapshot |
Support for Food System Firms that hire Temporary Foreign Workers (2020 Snapshot) |
50 | - | 50 | - | - | - | - | - | Policy Action Included in the July 2020 Snapshot |
| Extension of the Mandatory Isolation Support for Temporary Foreign Workers Program | 34 | - | 34 | - | - | - | - | - | New in this Fall Economic Statement |
| Addressing the Outbreak of COVID-19 among Temporary Foreign Workers on Farms | 59 | - | 59 | - | - | - | - | - | Policy Action Announced since the July 2020 Snapshot |
| 1.5 Long-Term Care | 1,340 | - | 823 | 516 | 1 | - | - | - | |
| Canadian Armed Forces Support for the COVID-19 Response | 418 | - | 417 | 0 | 0 | - | - | - | Policy Action Announced since the July 2020 Snapshot |
| Less: Funds Sourced from Existing Departmental Resources | -126 | - | -126 | - | - | - | - | - | Policy Action Announced since the July 2020 Snapshot |
| Addressing Labour Shortages in Long-Term and Home Care | 38 | - | 25 | 13 | - | - | - | - | Policy Action Announced since the July 2020 Snapshot |
| Further Investments in Long-Term Care | 1,010 | - | 506 | 503 | 1 | - | - | - | New in this Fall Economic Statement |
| 1.6.1 Mental Health and Virtual Care | 334 | - | 334 | - | - | - | - | - | |
| Virtual Care and Mental Health Support (2020 Snapshot) | 241 | - | 241 | - | - | - | - | - | Policy Action Included in the July 2020 Snapshot |
| Supporting Distress Centres and the Wellness Together Canada Portal | 93 | - | 93 | - | - | - | - | - | New in this Fall Economic Statement |
| 1.6.2 Fighting the Opioid Crisis | 66 | - | 21 | 45 | - | - | - | - | |
| Supporting Canadians struggling with Substance Use Disorder | 66 | - | 21 | 45 | - | - | - | - | New in this Fall Economic Statement |
| 1.6.4 Supporting the Canadian Red Cross’ Response to COVID-19 | 219 | - | 135 | 84 | 66 | - | - | - | |
| Support for the Canadian Red Cross (2020 Snapshot) | 100 | - | 100 | - | - | - | - | - | Policy Action Included in the July 2020 Snapshot |
| Further Support for the Canadian Red Cross' Response to COVID-19 | 35 | - | 35 | - | - | - | - | - | New in this Fall Economic Statement |
| Civilian Humanitarian Workforce (Red Cross) | 84 | - | - | 84 | 66 | - | - | - | New in this Fall Economic Statement |
| 1.6.6 Continuing to Support the Health Response in Indigenous Communities | 1,187 | - | 964 | 218 | 1 | 1 | 1 | 1 | |
Enhancing Public Health Measures in Indigenous Communities (2020 Snapshot) |
285 | 279 | 1 | 1 | 1 | 1 | 1 | Policy Action Included in the July 2020 Snapshot | |
| Further Enhancing Public Health Measures in Indigenous Communities | 632 | - | 537 | 94 | - | - | - | - | New in this Fall Economic Statement |
Indigenous Mental Wellness Support |
83 | - | 83 | - | - | - | - | - | Policy Action Announced since the July 2020 Snapshot |
| Supportive Care in Indigenous Communities | 187 | - | 64 | 123 | - | - | - | - | New in this Fall Economic Statement |
| 1.7 Contributing on the Global Stage | 845 | -179 | 702 | - | - | - | - | - | |
| Support for international partners (including $322.4 million of International Assistance Envelope Crisis Pool and other re-allocated funding) (2020 Snapshot) | 442 | -179 | 299 | - | - | - | - | - | Policy Action Included in the July 2020 Snapshot |
| Additional support for the international response to COVID-19 | 403 | - | 403 | - | - | - | - | - | Policy Action Announced since the July 2020 Snapshot |
| Other measures in the 2020 Snapshot | 1,781 | 561 | 1,146 | 83 | 40 | 40 | 40 | 40 | |
Immediate Public Health Response |
50 | 25 | 25 | - | - | - | - | - | Policy Action Included in the July 2020 Snapshot |
| COVID-19 Response Fund (including $500M for Provinces and Territories, completed in 2019-20 and $50M from existing resources) | 1,025 | 500 | 512 | 37 | 37 | 37 | 37 | 37 | Policy Action Included in the July 2020 Snapshot |
| Support for Health Canada and the Public Health Agency of Canada | 88 | - | 70 | 3 | 3 | 3 | 3 | 3 | Policy Action Included in the July 2020 Snapshot |
| Reducing Import Costs to facilitate access to Critical Medical Goods3 | Policy Action Included in the July 2020 Snapshot | ||||||||
Estimated Cost in 2020 Snapshot |
281 | - | 281 | 26 | - | - | - | - | Policy Action Included in the July 2020 Snapshot |
Re-Estimated Cost |
518 | - | 475 | 43 | - | - | - | - | Policy Action Included in the July 2020 Snapshot |
Difference |
237 | - | 194 | 17 | - | - | - | - | Policy Action Included in the July 2020 Snapshot |
Consular Assistance for Canadians Abroad |
100 | 36 | 64 | - | - | - | - | - | Policy Action Included in the July 2020 Snapshot |
| Total – | |||||||||
Policy Actions in the 2020 Snapshot |
20,453 | 582 | 19,106 | 467 | 48 | 48 | 48 | 48 | Policy Action Included in the July 2020 Snapshot |
Impact of re-estimated costs |
237 | - | 194 | 17 | - | - | - | - | Policy Action Announced since the July 2020 Snapshot |
Policy Actions since the 2020 Snapshot |
24,292 | - | 17,549 | 6,456 | 333 | 228 | 124 | 111 | Policy Action Announced since the July 2020 Snapshot |
| New Investments in Chapter 1 – Fighting COVID-19 | 7,538 | - | 3,565 | 3,951 | 301 | 118 | 9 | 9 | New in this Fall Economic Statement |
| Total – COVID-19 Economic Response Plan – Protecting Health and Safety |
52,520 | 582 | 40,414 | 10,892 | 682 | 394 | 181 | 168 | |
| Note: Numbers may not add due to rounding. 1 The impact value reflects projected cash expenditures and liquidity support primarily in 2020-21 (some measures also include 2019-20 expenditures, and projected expenditures in 2021-22). The fiscal (budgetary) impact on an accrual basis is lower, owing to cash-accrual accounting differences, the fact that some of these measures relate to loans, for which only provisions for potential losses would impact the balance, and tax deferrals, for which only foregone interest and penalties would affect the balance. 2 Spending profile adjusted to reflect updated departmental requirements. 3 Estimate assumes tariff waiver would remain in place for twelve months and may require adjustment based on the total duration of the measure. Estimated fiscal impact revised in September 2020 to reflect higher uptake than anticipated. |
|||||||||
Report a problem on this page
- Date modified: